6. Swiss Lymphsymposium
The 6. Swiss Lymphsymposium has just completed. This symposium seems to gain popularity with every iteration, and I heard that there was a waiting list this year. The Juzo AG had invited experts to discuss topics at the intersection of Edema and Adipositas. The meeting was interesting and did not shy away from controversies. For a bench scientist like me, it is always stimulating to get the healthcare practitioners' perspective into the diseases whose molecular basis I research. I had been at the 3. Swiss Lymphsymposium in 2021, and there have been many developments that I have chosen not to pay attention to in my ivory tower of basic biomedical research. Specifically, the new S2k lipedema guidelines which are in effect since the beginning of 2024 received lots of attention.
The new lipedema guidelines consider questions and goals related to diagnostic criteria, differential diagnostics, how diagnosis and therapy are influenced by co-morbidities, what therapeutic possibilities exist, and how patients can actively contribute to managing the disease. Given how little we understand about the etiology of lymphedema, these goals are ambitious. Dr. Tobias Bertsch from the Földi Clinic gave a very passionate and persuasive talk about the progress these guidelines represent in his talk "The New Guidelines Concerning the Lipedema Syndrome - More Light Than Shadow". The presentation loosely followed the position paper he published with many other European experts. The one item where the position paper deviates most from the guidelines is the evaluation of liposuction as a treatment option. The position paper clearly states that liposuction does not produce long-lasting results, whereas the guidelines are surprisingly sparse-worded about this topic, and the reached consensus received the lowest support from the authors among all recommendations.
For a bench scientist, making decisions absent high-grade evidence remains unsatisfying. However, guidelines for healthcare professionals cannot speak the same language as scientific articles because that would counteract their usefulness. "Whoever heals is right", and if the new guidelines result in better medical outcomes, they serve their purpose. Guidelines - as scientific knowledge - are always provisional and subject to adjustment once better evidence becomes available. At the same time, we have to be careful not to block progress by taking them as gospel. After all, the saying "Whoever heals is right" is attributed to Samuel Hahnemann, the German physician who founded homeopathy (which is essentially witchcraft; do I need to mention this?). Nevertheless, when Samuel Hahnemann lived, using homeopathy likely resulted in better medical outcomes than the mainstream treatments of the time, such as bloodletting or patent mercury potions, which were frequently not only useless but dangerous or toxic.
How I view lipedema
After following the lipedema field for a few years, my hypothesis is that lipedema is one endpoint in the wide spectrum of human fat storage physiology. Fat storage has been such a big asset during 99.999997% of evolution that nature was willing to accept the many risks inherent to complex and difficult systems. The more complex a machine, the more frequently it will fail, and many hereditary lipid-related diseases are failures of this machinery. The essential problem that this complex machinery has evolved to overcome is the insolubility of fat in water. Any transport of fat inside and outside the cell requires rendering fat water-soluble. In the blood, this is achieved by packaging fat molecules into lipoprotein particles.
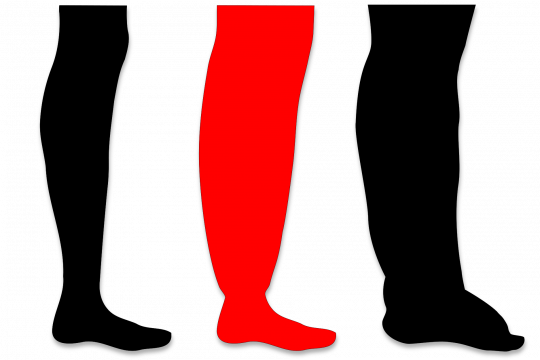
Lipids that are not burned get stored somewhere. They can be stored subcutaneously or viscerally. There are more ways to store fat, but this is the simplified version: Everybody will have a slightly different distribution between visceral and subcutaneous fat storage based on a complex interplay of many genes and the environment. In some people, this interplay results in extreme imbalances between these two compartments with pathological consequences. For example, in coronary heart disease, for most people, the genetic burden results from many genes (polygenic), whereas in a minority of patients, one or a few genes might explain the condition (monogenic or oligogenic). Hunting genes likely won't result in any actionable findings for most lipedema patients. However, similar to coronary artery disease, it might be possible to identify risk factors. We already know three risk factors for lipedema: being female, undergoing hormonal changes, and having a family history of the disease. It would be helpful to identify additional risk factors that are easier to modify than the three we know of. We need for lipedema something similar to what the blood lipid panel is for coronary heart disease. Here is the link to my presentation (which I will keep updating over time with better information): What do we really know about lipedema?. You can also download the German version Was wissen wir eigentlich sicher über Lipödeme? - Eine Bestandsaufnahme".



